Pancreatic Disease/Acute Pancreatitis, Chronic Pancreatitis
Dr. Amit Miglani
Senior Gastroenterologist, Hepatologist & Endoscopist of Faridabad.
Chronic pancreatitischaracterized by chronic and irreversible damage to the pancreas. Chronic inflammation of the pancreas leads to damage to the acinar cells which result in exocrine deficiency in the form of malabsorption of nutrients and loss of islet of langerhans cells which result in endocrine deficiency resulting in diabetes mellitus. Chronic pancreatitis can have varied presentation from asymptomatic to symptoms in the form of abdominal pain, steatorrhea( Fat Malabsorption) ,weight loss and Diabetes mellitus. More than 90% of the pancreas is damaged for symptoms to occur. CP is more common in middle aged men above 40 years of age and results in significant mortality and morbidity. The prognosis of CP is mainly driven by the underlying ongoing alcohol intake and also the increasing age, smoking, diabetes mellitus and chronic kidney disease.
Pathogenesis
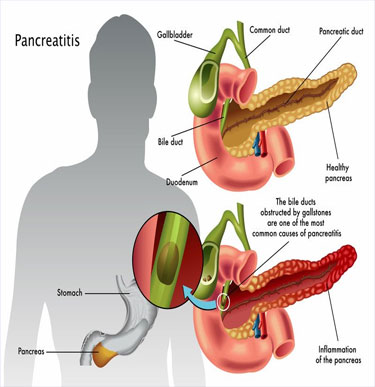
Chronic pancreatitis results due to the damage to the pancreas due to various factors. Due to chronic alcohol intake there is damage to the acinar cells which leads to release of various oxidants and free radicals. Alcohol is metabolized by pancreas by alternate pathway and leads to the formation of fatty acid ethanol esters (FAEE)which have direct cytotoxic effect on the acinar cells resulting in increased permeability of the ductal cells, leading to increased influx of calcium in the acinar cells followed by recruitment of neutrophils which results in injury and fibrosis of the gland. There is also increased secretion of pancreatic juice rich in protein with reduced bicarbonate secretion. As a result the Pancreatic duct gets blocked and there is formation of protein precipitates which calcify resulting in the formation of calculi within the PD which leads to parenchymal and ductal cell injury. Various genetic mutations CFTR,SPINK1,CFTR and environmental factors have been implicated in chronic pancreatitis .
ETIOLOGY
The most common cause is alcohol consumption. Alcohol has been associated with 40% of risk factors for chronic pancreatitis. Chronic alcohol intake for around 4 to 5 drinks per day for a duration or at least 5 to 10 years have been seen to result in chronic pancreatitis . Men are more likely than women to develop chronic pancreatitis. However only 2% to 5% of chronic alcoholics develop CP suggesting the role of other cofactors in the disease progression like genetic factors and environmental factors.
Smoking has been seen as an independent risk factor for Chronic pancreatitis. Smoking with alcohol intake is strongly associated with CP.
Tropical pancreatitis most common in South India is mostly in youth and early adulthood with mean age of onset before 24 years.
Genetic factors mutations in PRSS1 gene, SPINK1 and CFTR gene mutations
Autoimmune pancreatitis
CLINICAL FEATURES
Abdominal pain is the most common presentation .Pain is most commonly located in the epigastrium boring deep and penetrating with radiation to the back and relieved on sitting or leaning forwards. Pain is associated with decreased appetite which results in reduced calorie intake causing weight loss and malnutrition. Patients may present with acute exacerbation of pain interspersed with pain free intervals.
Steatorrhea: When lipase secretion is reduced to <10% patients have diarrhea and weight loss with bulky foul smelling stools of passage of oil droplets with the stools resulting due to fat maldigestion.
Diabetes mellitus due to endocrine insufficiency known as pancreatogenic diabetes or type 3C diabetes. There are low levels of insulin and glucagon levels and is difficult to treat and frequently leads to treatment induced hypoglycemia.
On Examination the patient will appear undernourished with mild to moderate abdominal tenderness. Splenomegaly can be present due to splenic vein thrombosis secondary to chronic pancreatitis. Pseudocyst may be palpable in some cases. Jaundice may be present due to underlying alcoholic liver disease or may be secondary to bile duct compression in the head of pancreas.
Diagnosis
Chronic pancreatitis is a slowly progressive disease which takes several years to manifest. As pancreas has both endocrine and exocrine functions so diagnosis is mainly based on decrease in the secretion of various enzymes secreted by pancreas.
Tests of exocrine function are direct tests in which the pancreatic secretions are collected from duodenum by placement of a tube which analyses the bicarbonate concentration and various enzymes secreted by pancreas in the pancreatic juice.
Indirect tests measure the serum levels of trypsinogen, measurement of fecal chymotrypsin and elastase-1 levels which are reduced in CP. Fecal fat excretion of > 7gm in a 72 hour collected stool sample is suggestive of fat maldigestion.
Tests for pancreatic structure
X Ray abdomen shows calcification in the pancreatic area
Ultrasound of the abdomen may show PD dilatation, calculi in the PD, gland irregularity, Pancreatic atrophy and pseudocyst and changes in pancreatic parenchymal echotexture. Ultrasound has a sensitivity of 50% to 60% in CP with an overall accuracy of 56%.CT Scan of Abdomen is a more specific and sensitive test for detection of Chronic Pancreatitis changes about 85% to 90%.MRI with MRCP is also a very specific test which detects changes in the main Pancreatic Duct and side branches and can detect early signs of Chronic Pancreatitis . ERCP can be helpful in diagnosis which detects abnormalities in the PD and side branches. Endoscopic Ultrasound (EUS) is more specific test in Chronic Pancreatitis and classifies CP according to various classification systems such as Rosemont criteria in which detection of abnormalities of the Pancreatic Duct, parenchyma,lobularity of the gland and ductal calcification can be assessed.
Treatment
Abdominal pain is the most common presenting complaint which results in major morbidity so the management of abdominal pain is important to improve the quality of life. Initially simple analgesics like NSAIDS should be used. If the patient does not respond to simple analgesics and opioid analgesics are used. Other adjuncts can be used like tricyclic antidepressants, SSRI’S, serotonin norepinephrine reuptake inhibitors like duloxetine, gabapentin or pregabalin. Underlying cause of pain is to be assessed with cross sectional imaging. Pseudocyst, Pancreatic Duct stricture or duodenal obstruction should be looked for. Cessation of alcohol should be advised. Antioxidants to reduce the oxidative stress injury. Pancreatic enzymes which activate the duodenal feedback and reduce pancreatic ductal pressure and pain. Endoscopic therapy to drain any
pseudocyst or placement of PD stent in case of stricture in PD or removal of PD calculi. EUS guided celiac plexus block with glucocorticoids and long acting anesthetic or neurolysis with absolute alcohol. Surgical resection can be considered for patients not responding to medical therapy. Stetorrhoea can be treated by replacement of pancreatic enzymes with each major meal. Supplementation of fat soluble vitamins in case of their deficiency.